
hehehehe...see stuff ooo......Yellow fever is an acute viral disease. In most cases, symptoms include fever, chills, loss of appetite, nausea, muscle pains particularly in the back, and headaches. Symptoms typically improve within five days. In some people within a day of improving, the fever comes back, abdominal pain occurs, and liver damage begins causing yellow skin. If this occurs, the risk of bleeding and kidney problems is also increased.
The disease is caused by the yellow fever virus and is spread by the bite of an infected female mosquito. It infects only humans, other primates, and several species of mosquitoes. In cities, it is spread primarily by mosquitoes of the Aedes aegypti species. The virus is an RNA virus of the genus Flavivirus. The disease may be difficult to tell apart from other illnesses, especially in the early stages. To confirm a suspected case, blood sample testing with polymerase chain reaction is required.
A safe and effective vaccine against yellow fever exists and some countries require vaccinations for travelers. Other efforts to prevent infection include reducing the population of the transmitting mosquito. In areas where yellow fever is common and vaccination is uncommon, early diagnosis of cases and immunization of large parts of the population is important to prevent outbreaks. Once infected, management is symptomatic with no specific measures effective against the virus. The second and more severe phase results in death in up to half of people without treatment.
Yellow fever causes 200,000 infections and 30,000 deaths every year, with nearly 90% of these occurring in Africa. Nearly a billion people live in an area of the world where the disease is common. It is common in tropical areas of South America and Africa, but not in Asia. Since the 1980s, the number of cases of yellow fever has been increasing.[3][8] This is believed to be due to fewer people being immune, more people living in cities, people moving frequently, and changing climate. The disease originated in Africa, from where it spread to South America through the slave trade in the 17th century.Since the 17th century, several major outbreaks of the disease have occurred in the Americas, Africa, and Europe. In the 18th and 19th centuries, yellow fever was seen as one of the most dangerous infectious diseases. In 1927 yellow fever virus became the first human virus to be isolated.
Signs and symptoms
Yellow fever begins after an incubation period of three to six days. Most cases only cause a mild infection with fever, headache, chills, back pain, fatigue, loss of appetite, muscle pain, nausea, and vomiting. In these cases, the infection lasts only three to four days.In 15 percent of cases, however, people enter a second, toxic phase of the disease with recurring fever, this time accompanied by jaundice due to liver damage, as well as abdominal pain. Bleeding in the mouth, the eyes, and the gastrointestinal tract will cause vomit containing blood, hence the Spanish name for yellow fever, vomito negro ("black vomit"). There may also be kidney failure, hiccups, and delirium.
The toxic phase is fatal in about 20 to 50 percent of cases, making the overall fatality rate for the disease about 3.0 to 7.5 percent. However, the fatality rate of those with the toxic phase of the disease may exceed 50%.
Surviving the infection provides lifelong immunity, and normally there is no permanent organ damage.
Cause
| Yellow fever virus | |
|---|---|
| Virus classification | |
| Group: | Group IV ((+)ssRNA) |
| Order: | Unassigned |
| Family: | Flaviviridae |
| Genus: | Flavivirus |
| Species: | Yellow fever virus |
The viruses infect, amongst others, monocytes, macrophages, and dendritic cells. They attach to the cell surface via specific receptors and are taken up by an endosomal vesicle. Inside the endosome, the decreased pH induces the fusion of the endosomal membrane with the virus envelope. The capsid enters the cytosol, decays, and releases the genome. Receptor binding, as well as membrane fusion, are catalyzed by the protein E, which changes its conformation at low pH, causing a rearrangement of the 90 homodimers to 60 homotrimers.
After entering the host cell, the viral genome is replicated in the rough endoplasmic reticulum (ER) and in the so-called vesicle packets. At first, an immature form of the virus particle is produced inside the ER, whose M-protein is not yet cleaved to its mature form and is therefore denoted as prM (precursor M) and forms a complex with protein E. The immature particles are processed in the Golgi apparatus by the host protein furin, which cleaves prM to M. This releases E from the complex which can now take its place in the mature, infectious virion.
Transmission
Aedes aegypti feeding

Adults of the yellow fever mosquito A. aegypti: The male is on the left, females are on the right. Only the female mosquito bites humans to transmit the disease.
Three epidemiologically different infectious cycles occur, in which the virus is transmitted from mosquitoes to humans or other primates. In the "urban cycle", only the yellow fever mosquito A. aegypti is involved. It is well adapted to urban areas and can also transmit other diseases, including Zika fever, dengue fever and chikungunya. The urban cycle is responsible for the major outbreaks of yellow fever that occur in Africa. Except in an outbreak in 1999 in Bolivia, this urban cycle no longer exists in South America.
Besides the urban cycle, both in Africa and South America, a sylvatic cycle (forest cycle or jungle cycle) is present, where Aedes africanus (in Africa) or mosquitoes of the genus Haemagogus and Sabethes (in South America) serve as vectors. In the jungle, the mosquitoes infect mainly non-human primates; the disease is mostly asymptomatic in African primates. In South America, the sylvatic cycle is currently the only way humans can become infected, which explains the low incidence of yellow fever cases on the continent. People who become infected in the jungle can carry the virus to urban areas, where A. aegypti acts as a vector. Because of this sylvatic cycle, the yellow fever cannot be eradicated.
In Africa, a third infectious cycle known as "savannah cycle" or intermediate cycle, occurs between the jungle and urban cycles. Different mosquitoes of the genus Aedes are involved. In recent years, this has been the most common form of transmission of yellow fever in Africa.
There is concern about yellow fever spreading to southeast Asia, where its vector Aedes aegypti already occurs.
Pathogenesis
After transmission from a mosquito, the viruses replicate in the lymph nodes and infect dendritic cells in particular. From there, they reach the liver and infect hepatocytes (probably indirectly via Kupffer cells), which leads to eosinophilic degradation of these cells and to the release of cytokines. Apoptotic masses known as Councilman bodies appear in the cytoplasm of hepatocytes.Fatality may occur when cytokine storm, shock, and multiple organ failure follow.
Diagnosis
Yellow fever is a clinical diagnosis, which often relies on the whereabouts of the diseased person during the incubation time. Mild courses of the disease can only be confirmed virologically. Since mild courses of yellow fever can also contribute significantly to regional outbreaks, every suspected case of yellow fever (involving symptoms of fever, pain, nausea and vomiting six to 10 days after leaving the affected area) is treated seriously.If yellow fever is suspected, the virus cannot be confirmed until six to 10 days after the illness. A direct confirmation can be obtained by reverse transcription polymerase chain reaction where the genome of the virus is amplified. Another direct approach is the isolation of the virus and its growth in cell culture using blood plasma; this can take one to four weeks.
Serologically, an enzyme linked immunosorbent assay during the acute phase of the disease using specific IgM against yellow fever or an increase in specific IgG-titer (compared to an earlier sample) can confirm yellow fever. Together with clinical symptoms, the detection of IgM or a fourfold increase in IgG-titer is considered sufficient indication for yellow fever. Since these tests can cross-react with other flaviviruses, like dengue virus, these indirect methods cannot conclusively prove yellow fever infection.
Liver biopsy can verify inflammation and necrosis of hepatocytes and detect viral antigens. Because of the bleeding tendency of yellow fever patients, a biopsy is only advisable post mortem to confirm the cause of death.
In a differential diagnosis, infections with yellow fever must be distinguished from other feverish illnesses like malaria. Other viral hemorrhagic fevers, such as Ebola virus, Lassa virus, Marburg virus, and Junin virus, must be excluded as cause.
Prevention
Personal prevention of yellow fever includes vaccination, as well as avoidance of mosquito bites in areas where yellow fever is endemic. Institutional measures for prevention of yellow fever include vaccination programmes and measures of controlling mosquitoes. Programmes for distribution of mosquito nets for use in homes are providing reductions in cases of both malaria and yellow fever.Vaccination
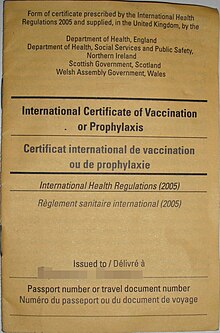
The cover of a certificate that confirms the holder has been vaccinated against yellow fever
Main article: Yellow fever vaccine
Vaccination
is recommended for those traveling to affected areas, because
non-native people tend to suffer more severe illness when infected.
Protection begins by the 10th day after vaccine administration in 95% of
people, and lasts for at least 10 years. About 81% of people are still immune
after 30 years. The attenuated live vaccine stem 17D was developed in
1937 by Max Theiler. The World Health Organization (WHO) recommends routine vaccinations for people living in affected areas between the ninth and 12th month after birth. Up to one in four people experience fever, aches, and local soreness and redness at the site of injection.In rare cases (less than one in 200,000 to 300,000), the vaccination can cause yellow fever vaccine-associated viscerotropic disease, which is fatal in 60% of cases. It is probably due to the genetic morphology of the immune system. Another possible side effect is an infection of the nervous system, which occurs in one in 200,000 to 300,000 cases, causing yellow fever vaccine-associated neurotropic disease, which can lead to meningoencephalitis and is fatal in less than 5% of cases.
In 2009, the largest mass vaccination against yellow fever began in West Africa, specifically Benin, Liberia, and Sierra Leone. When it is completed in 2015, more than 12 million people will have been vaccinated against the disease. According to the WHO, the mass vaccination cannot eliminate yellow fever because of the vast number of infected mosquitoes in urban areas of the target countries, but it will significantly reduce the number of people infected.[ The WHO plans to continue the vaccination campaign in another five African countries — the Central African Republic, Ghana, Guinea, Ivory Coast, and Nigeria — and stated that about 160 million people in the continent could be at risk unless the organization acquires additional funding to support widespread vaccinations.[34]
In 2013, the WHO stated, "a single dose of vaccination is sufficient to confer life-long immunity against yellow fever disease."
Compulsory vaccination
Some countries in Asia are theoretically in danger of yellow fever epidemics (mosquitoes with the capability to transmit yellow fever and susceptible monkeys are present), although the disease does not yet occur there. To prevent introduction of the virus, some countries demand previous vaccination of foreign visitors if they have passed through yellow fever areas. Vaccination has to be proven in a vaccination certificate which is valid 10 days after the vaccination and lasts for 10 years. Although the WHO on 17 May 2013 advised that subsequent booster vaccinations are unnecessary, an older (than 10 years) certificate may not be acceptable at all border posts in all affected countries. A list of the countries that require yellow fever vaccination is published by the WHO.[36] If the vaccination cannot be conducted for some reasons, dispensation may be possible. In this case, an exemption certificate issued by a WHO-approved vaccination center is required. Although 32 of 44 countries where yellow fever occurs endemically do have vaccination programmes, in many of these countries, less than 50% of their population is vaccinated.[5]Vector control
Control of the yellow fever mosquito A. aegypti is of major importance, especially because the same mosquito can also transmit dengue fever and chikungunya disease. A. aegypti breeds preferentially in water, for example in installations by inhabitants of areas with precarious drinking water supply, or in domestic waste; especially tires, cans, and plastic bottles. These conditions are common in urban areas in developing countries.Two main strategies are employed to reduce mosquito populations. One approach is to kill the developing larvae. Measures are taken to reduce the water accumulations in which the larva develops. Larvicides are used, as well as larvae-eating fish and copepods, which reduce the number of larvae. For many years, copepods of the genus Mesocyclops have been used in Vietnam for preventing dengue fever. It eradicated the mosquito vector in several areas. Similar efforts may be effective against yellow fever. Pyriproxyfen is recommended as a chemical larvicide, mainly because it is safe for humans and effective even in small doses.[5]
The second strategy is to reduce populations of the adult yellow fever mosquito. Lethal ovitraps can reduce Aedes populations, but with a decreased amount of pesticide because it targets the mosquitoes directly. Curtains and lids of water tanks can be sprayed with insecticides, but application inside houses is not recommended by the WHO. Insecticide-treated mosquito nets are effective, just as they are against the Anopheles mosquito that carries malaria.[5]
Treatment
As for other flavivirus infections, no cure is known for yellow fever. Hospitalization is advisable and intensive care may be necessary because of rapid deterioration in some cases.
Endemic range of yellow fever in South America (2009)
Endemic range of yellow fever in Africa (2009)
Worldwide, about 600 million people live in endemic areas. The WHO estimates 200,000 cases of disease and 30,000 deaths a year occur; the number of officially reported cases is far lower. An estimated 90% of the infections occur on the African continent.[5] In 2008, the largest number of recorded cases were in Togo.
Phylogenetic analysis identified seven genotypes of yellow fever viruses, and they are assumed to be differently adapted to humans and to the vector A. aegypti. Five genotypes (Angola, Central/East Africa, East Africa, West Africa I, and West Africa II) occur only in Africa. West Africa genotype I is found in Nigeria and the surrounding areas.[44] This appears to be especially virulent or infectious, as this type is often associated with major outbreaks. The three genotypes in East and Central Africa occur in areas where outbreaks are rare. Two recent outbreaks in Kenya (1992–1993) and Sudan (2003 and 2005) involved the East African genotype, which had remained unknown until these outbreaks occurred.[45]






No comments:
Post a Comment