Hehehe...see stuff oooo....Diabetes mellitus (DM), commonly referred to as diabetes, is a group of metabolic diseases in which there are high blood sugar levels over a prolonged period. Symptoms of high blood sugar include frequent urination, increased thirst, and increased hunger. If left untreated, diabetes can cause many complications. Acute complications include diabetic ketoacidosis and nonketotic hyperosmolar coma. Serious long-term complications include cardiovascular disease, stroke, chronic kidney failure, foot ulcers, and damage to the eyes.
Diabetes is due to either the pancreas not producing enough insulin or the cells of the body not responding properly to the insulin produced. There are three main types of diabetes mellitus:
- Type 1 DM results from the pancreas's failure to produce enough insulin. This form was previously referred to as "insulin-dependent diabetes mellitus" (IDDM) or "juvenile diabetes". The cause is unknown.
- Type 2 DM begins with insulin resistance, a condition in which cells fail to respond to insulin properly. As the disease progresses a lack of insulin may also develop.[6] This form was previously referred to as "non insulin-dependent diabetes mellitus" (NIDDM) or "adult-onset diabetes". The primary cause is excessive body weight and not enough exercise.
- Gestational diabetes, is the third main form and occurs when pregnant women without a previous history of diabetes develop high blood-sugar levels.
e 2 DM may be treated with medications with or without insulin. Insulin and some oral medications can cause low blood sugar. Weight loss surgery in those with obesity is sometimes an effective measure in those with type 2 DM. Gestational diabetes usually resolves after the birth of the baby.
As of 2015, an estimated 415 million people have diabetes worldwide,[11] with type 2 DM making up about 90% of the cases. This represents 8.3% of the adult population,[13] with equal rates in both women and men. From 2012 to 2015, diabetes is estimated to have resulted in 1.5 to 5.0 million deaths each year. Diabetes at least doubles a person's risk of death.The number of people with diabetes is expected to rise to 592 million by 2035.The global economic cost of diabetes in 2014 was estimated to be $612 billion USD. In the United States, diabetes cost $245 billion in 2012.
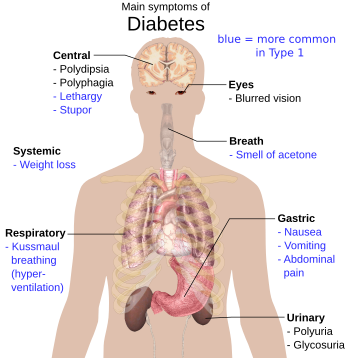
The classic symptoms of untreated diabetes are weight loss, polyuria (increased urination), polydipsia (increased thirst), and polyphagia (increased hunger).[18] Symptoms may develop rapidly (weeks or months) in type 1 DM, while they usually develop much more slowly and may be subtle or absent in type 2 DM.
Several other signs and symptoms can mark the onset of diabetes, although they are not specific to the disease. In addition to the known ones above, they include blurry vision, headache, fatigue, slow healing of cuts, and itchy skin. Prolonged high blood glucose can cause glucose absorption in the lens of the eye, which leads to changes in its shape, resulting in vision changes. A number of skin rashes that can occur in diabetes are collectively known as diabetic dermadromes.
Diabetic emergencies
Low blood sugar is common in persons with type 1 and type 2 DM. Most cases are mild and are not considered medical emergencies. Effects can range from feelings of unease, sweating, trembling, and increased appetite in mild cases to more serious issues such as confusion, changes in behavior, seizures, unconsciousness, and (rarely) permanent brain damage or death in severe cases.[19][20] Mild cases are self-treated by eating or drinking something high in sugar. Severe cases can lead to unconsciousness and must be treated with intravenous glucose or injections with glucagon.People (usually with type 1 DM) may also experience episodes of diabetic ketoacidosis, a metabolic disturbance characterized by nausea, vomiting and abdominal pain, the smell of acetone on the breath, deep breathing known as Kussmaul breathing, and in severe cases a decreased level of consciousness.[21]
A rare but equally severe possibility is hyperosmolar nonketotic state, which is more common in type 2 DM and is mainly the result of dehydration.
Complications
The major long-term complications relate to damage to blood vessels. Diabetes doubles the risk of cardiovascular disease and about 75% of deaths in diabetics are due to coronary artery disease. Other "macrovascular" diseases are stroke, and peripheral vascular disease.
The primary complications of diabetes due to damage in small blood vessels include damage to the eyes, kidneys, and nerves. Damage to the eyes, known as diabetic retinopathy, is caused by damage to the blood vessels in the retina of the eye, and can result in gradual vision loss and blindness. Damage to the kidneys, known as diabetic nephropathy, can lead to tissue scarring, urine protein loss, and eventually chronic kidney disease, sometimes requiring dialysis or kidney transplant. Damage to the nerves of the body, known as diabetic neuropathy, is the most common complication of diabetes. The symptoms can include numbness, tingling, pain, and altered pain sensation, which can lead to damage to the skin. Diabetes-related foot problems (such as diabetic foot ulcers) may occur, and can be difficult to treat, occasionally requiring amputation. Additionally, proximal diabetic neuropathy causes painful muscle wasting and weakness.
There is a link between cognitive deficit and diabetes. Compared to those without diabetes, those with the disease have a 1.2 to 1.5-fold greater rate of decline in cognitive function
y, and why keeping an eye on your levels is essential to diabetes management »
Type 1 Medications
Type 1 diabetes, once called
juvenile diabetes, is normally present from childhood. Lacking proper insulin
can cause people with this type of diabetes to experience unbalanced blood glucose
levels. According to the Mayo Clinic,
healthy blood glucose levels range from 70 to 130 milligrams per deciliter (mg/dL)
before meals. Since the body has problems processing glucose, medications are
needed to compensate for the lack of insulin.
Insulin
Insulin is the most common type of medication used in type 1 diabetes treatment. It is mostly administered through injections. Insulin is also used in type 2. The type of insulin you need depends on the severity of insulin depletion. Options include:- short-acting: regular (R) (Humulin, Novolin, and other brands)
- rapid-acting: insulin aspart (NovoLog, FlexPen), insulin glulisine (Apidra), insulin lispro (Humalog)
- intermediate-acting: insulin isophane (Humulin, Novolin, Iletin)
- long-acting: insulin detemir (Levemir), insulin glargine (Lantus)
Amylinomimetic
Pramlintide (SymlinPen 120, SymlinPen 60) delays the time it takes the stomach to empty. It reduces glucagon secretion after meals and reduces appetite through a central mechanism. It is used before meals.Other Medicines
Other recommended treatments may include:- aspirin for heart health
- cholesterol-lowering medication
- high blood pressure medication
Type 2 Medications
Type 2 diabetes happens when
the body becomes resistant to insulin. Although the exact cause is unknown,
it’s thought that both genetics and environmental factors, such as being
overweight, may be risks.
In type 2, over time, the pancreas may no longer make insulin, and the body might become resistant to it altogether. For this reason, insulin injections can play a role in type 2 treatment as well. However, there are other types of medications often recommended only for type 2.
Metformin can also be combined into a single medication with other type 2 medication types. It is included as an ingredient in:
In type 2, over time, the pancreas may no longer make insulin, and the body might become resistant to it altogether. For this reason, insulin injections can play a role in type 2 treatment as well. However, there are other types of medications often recommended only for type 2.
Alpha-Glucosidase Inhibitors
These medications help lower blood glucose by assisting the body with breaking down starchy foods and table sugar. For the best results, they’re taken before meals. Options include:Biguanides
Biguanides decrease glucose production in the liver. They decrease intestinal glucose absorption and increase insulin sensitivity. They also help muscles absorb glucose. The most common biguanide is metformin (Glucophage, Metformin Hydrochloride ER, Glumetza, Riomet, Fortamet).Metformin can also be combined into a single medication with other type 2 medication types. It is included as an ingredient in:
- metformin-alogliptin (Kazano)
- metformin-canagliflozin (Invokamet)
- metformin-glipizide
- metformin-glyburide (Glucovance)
- metformin-linagliptin (Jentadueto)
- metformin-pioglitazone (Actoplus)
- metformin-repaglinide (PrandiMet)
- metformin-rosiglitazone (Avandamet)
- metformin-saxagliptin (Kombiglyze XR)
- metformin-sitagliptin (Janumet)
- glyburide-metformin (Glucovance)
Dopamine Agonist
Action in diabetes is unknown, but bromocriptine (Parlodel) may affect circadian rhythms and affect obesity and insulin resistance.DPP-4 Inhibitors
DPP-4 inhibitors help the body preserve insulin production. They work by reducing blood glucose without causing hypoglycemia. These can also help the pancreas make more insulin. Options include:- alogliptin (Nesina)
- alogliptin and pioglitazone (Oseni)
- linagliptin (Tradjenta)
- saxagliptin (Onglyza)
- sitagliptin (Januvia)
- sitagliptin and simvastatin
Glucagon-Like Peptides
These are similar to the natural hormone incretin. They increase insulin secretion and decrease glucagon secretion. They also increase B-cell growth, slow stomach emptying, and reduce appetite. Options include:- albiglutide (Tanzeum)
- dulaglutide (Trulicity)
- exenatide (Byetta)
- liraglutide (Victoza)
Meglitinides
These medications stimulate insulin release. Unlike DPP-4 inhibitors, however, meglitinides may lower blood sugar. They are taken three times a day before meals. Options include: nateglinide (Starlix) and repaglinide (Prandin).SGLT2 Inhibitors
Sodium glucose transporter (SGLT) 2 inhibitors work by preventing the kidneys from holding onto glucose. Instead, SGLT2 promotes excretion through the urine. The forms of this medicine available are:- dapagliflozin (Farxiga)
- canagliflozin (Invokana)
- empagliflozin (Jardiance)
Sulfonylureas
These are among the oldest diabetes medications still used today. They work by stimulating the pancreas with the help of beta cells. In turn, more insulin is produced. Sulfonylureas come in the form of:- glimepiride (Amaryl)
- glimepiride and pioglitazone (Duetact)
- glimeperide and rosiglitazone (Avandaryl)
- gliclazide
- glipiZIDE (Glucotrol)
- glyBURIDE (DiaBeta, Glynase, Micronase)
- chlorproPAMIDE (Diabinese)
- TOLAZamide (Tolinase)
- TOLBUTamide (Orinase, Tol-Tab)


No comments:
Post a Comment